Case Studies: Partnering with a 3rd Party Vendor for Comprehensive Cardiac Device Clinic Management Solutions
How do Cardiology Clinics Benefit from Partnering with A Comprehensive Device Clinic Solutions Provider
Device clinics face the ever-growing challenge of managing patient loads efficiently, particularly in the realm of remote monitoring. This challenge underscores the need for innovative solutions that can streamline operations and enhance patient care without compromising on quality. This blog delves into some real-world case studies of how partnerships with a specialized third-party vendor, PrepMD, have revolutionized the management of cardiac device clinics.
This blog explores the journey of various clinics as they navigate the complexities of modern cardiac care. Through short case studies, we reveal how these clinics, by partnering with expert third-party vendors, have successfully integrated advanced remote management solutions into their practice. These partnerships not only address the logistical challenges of CIED remote monitoring but also bring a wealth of clinical expertise, technological innovation, and improved operational efficiency. As we delve into these cases, the benefits of such collaborations become clear, showcasing a path forward for clinics striving to excel in today’s fast-paced healthcare landscape.
Case Study 1: Large Cardiology Device Clinic Needs Additional Trained Staff to Remote Monitoring Workload
The Device Clinic Problem
A prominent device clinic recognized the strain on its resources, particularly in managing the burgeoning patient load requiring remote monitoring. The need for additional, well-trained staff became critical to maintain the high standard of patient care and manage the workload without overburdening existing staff or compromising on service quality.
The Solution Provided
After in-depth consultation to understand the clinic’s unique challenges, a tailored solution was crafted to address their challenges. The clinic opted for a bundled approach, leveraging the cost-effectiveness and expertise of PrepMD’s solutions. This comprehensive package included PrepMD’s remote monitoring services, along with access to PrepMD’s in-clinic staffing solutions. By integrating these services, the clinic was able to significantly enhance its operational capacity, ensuring that the increased demand for patient monitoring was met with a high degree of professionalism and care.
Case Study 2: A Large Device Clinic Utilizing A Different Remote Monitoring Software Needs Help with Staffing
The Device Clinic Problem
A well-established Device Clinic, previously utilizing software from a different provider, encountered significant hurdles in recruiting trained and experienced clinical staff to manage their remote monitoring load effectively. In their quest for a solution, the clinic reached out to PrepMD, known for their expertise in staffing and training in the cardiac device management sector.
The Solution Provided
In the course of our strategic discussions, the clinic recognized a comprehensive bundled solution not only addressed their staffing concerns but also delivered tech efficiencies. By bundling of PrepMD’s proprietary software with in-clinic staff solution, the clinic could substantially reduce their costs. This bundled approach was anchored by PrepMD’s robust hire-train-deploy-develop model, ensuring a continuous pipeline of skilled professionals. This software is designed for ease of use with a steep learning curve, which further streamlines clinic workflows and elevates the efficiency of patient management processes.
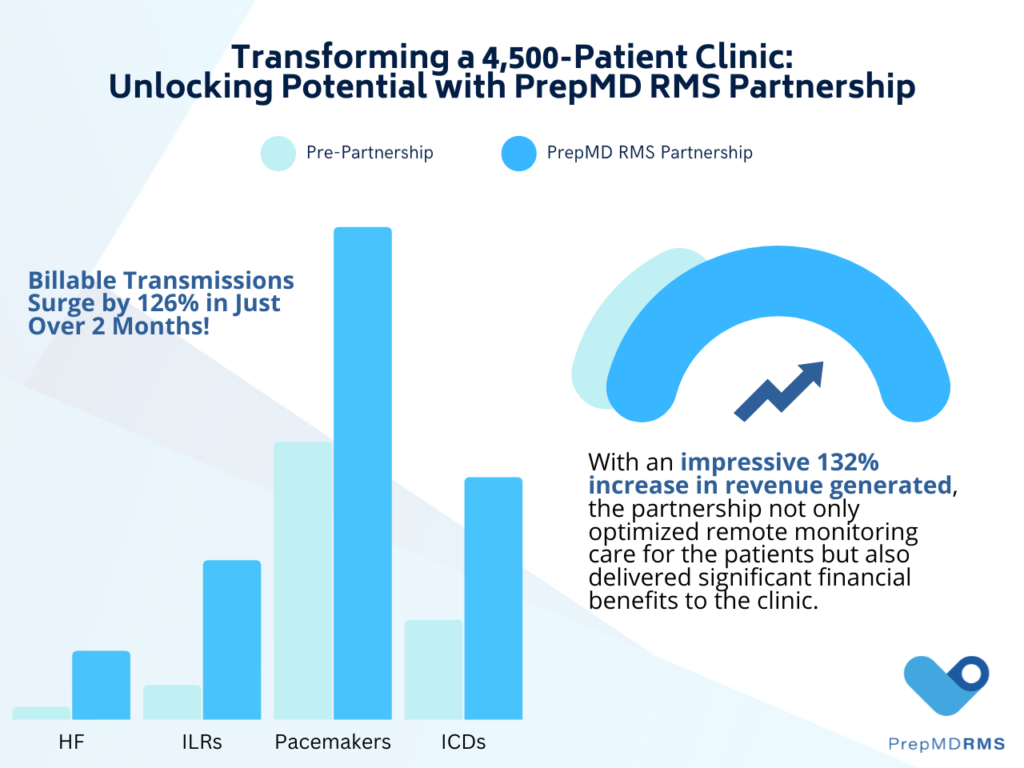
Case Study 3: A 4500+ Cardiac Patient Clinic with a Growing Remote Transmission Backlog Needs Help
The Device Clinic Problem
A 4500+ patient clinic needed a solution to better service their cardiac device patients. While alerts were being triaged, they had an ever-growing backlog of over 2,000 remote transmissions. Additional stressors included a newly hired staff who were overwhelmed with patient care and administrative responsibilities. All this led to regular CIED remote transmissions sometimes waiting weeks for review. The clinic leadership knew they needed help.
The Solution Provided
PrepMD worked tirelessly to clean up the clinic’s remote monitoring transmission backlog within 8 weeks, while also managing all daily scheduled and alert transmissions. This 4,500 cardiac patient clinic staff continues to rely on a dedicated PrepMD team of IBHRE® CCDS and CDRMS Certified Specialists for their expert clinical knowledge and a collaborative trusted approach, leading to the best outcomes for their patients.
Case Study 4: Large Network of Cardiology Clinics Needs Help Streamlining their Workflow
The Device Clinic Problem
A large healthcare network of cardiology clinics was unable to keep up with the sheer volume of remote monitoring transmissions. The network contained multiple cardiology clinics all operating under different work streams. The clinic leadership was seeking a solution to streamline their processes. As a result, regularly scheduled pacemaker, ICD and ILR remote reports were piling up at all clinics. This transmission backlog and clinic inefficiencies was leading to a very frustrated and overwhelmed clinic staff.
The Solution Provided
After meeting with the Nurse Manager and the clinic staff, the PrepMD team was able to find an integrative remote monitoring solution where we work with the clinic as partners. For example, our team led by IBHRE® Certified Cardiac Device Specialists customizes their service, making adjustments sometimes daily to the report writing and workflow. This allows us to seamlessly work within the protocols set by the clinic leadership. As such, we provided a solution to lessen their workflow burden and allow for prompt triaging and report writing for device transmissions.
Case Study 5: Cardiology Device Clinic Needs a Remote Monitoring Service Provider with a Stronger Alert Management Protocol
The Device Clinic Problem
A clinic was frustrated with the slow response to life threatening alerts from their previous remote monitoring service provider. Some high priority alerts from the previous service provider had not been delivered to the clinic for 2 months, leaving clinic staff frustrated. Additionally, patients were fearful that their devices were not monitored appropriately. As a result, the clinic was in search of a service provider with a tighter alert protocol procedure.
The Solution Provided
After consultation with the clinic we implemented a customized alert protocol to fit the clinic’s needs and expectations, therefore, never leaving the clinic staff or patients to worry about the monitoring of their device alerts again. This clinic wanted a service model they could trust and found it at PrepMD. Our service includes same-day alert reporting 5 days a week from a team lead by IBHRE® certified cardiac device specialists.
Case Study 6: Medium-Sized Cardiac Device Clinic Needed Report Writing Improvements for Easier Identification of Actionable Reports
The Device Clinic Problem
A medium-sized cardiac device clinic found itself falling behind with its remote CIED transmissions due to reporting inefficiencies. As a result, the clinical staff became overwhelmed because they struggled to write concise and clinically relevant reports. They wanted their reports written in a manner to easily identify actionable items to ensure the best patient care.
The Solution Provided
The PrepMD team worked with the cardiology clinic staff to implement a streamlined approach to remote report writing. Our IBHRE® certified cardiac device specialists craft reports which highlight the most important aspects of the transmissions. This approach not only allowed the doctors and staff to quickly review and assess reports, but also led to less actionable reports being missed.
Case Study 7: Cardiology Clinic Searching for a Remote Monitoring Service Provider to Ensure Billing and Reimbursement Accuracy
The Device Clinic Problem
A cardiology clinic needed guidance on a new workflow which would lead to more accurate billing to solve reimbursement issues. Therefore, the doctors were worried about a loss of revenue and had to put billing on hold until a solution could be found.
The Solution Provided
PrepMD was able to immediately implement a simple solution to ensure a proper billing workflow. As a result, the physicians at this clinic were able to receive the correct payment for remote reports on their cardiac device patients. The IBHRE® certified staff at PrepMD assigned a dedicated team to this clinic enabling a quick resolution so the clinic was able to resume billing very quickly.




 “Unfortunately, there is a lack of a unified approach to remote monitoring across the entire cardiac device remote monitoring space. This leads to confusion of what is needed to run a device remote monitoring program. There is an unfortunate tendency where this type of remote care can lead to a devaluing of the work being performed, simply because there is not a face-to-face patient interaction taking place, the value of the clinical care should not be minimized.” Jess Rizzo, CCDS,
“Unfortunately, there is a lack of a unified approach to remote monitoring across the entire cardiac device remote monitoring space. This leads to confusion of what is needed to run a device remote monitoring program. There is an unfortunate tendency where this type of remote care can lead to a devaluing of the work being performed, simply because there is not a face-to-face patient interaction taking place, the value of the clinical care should not be minimized.” Jess Rizzo, CCDS, 

 At a recent PrepMD Webinar a panel discussion was held to share best practices to address the common challenges on cardiac device remote monitoring programs. The panel discussion was led by Rob Lerman, MD, CMO, along with three CCDS-certificated leaders from the
At a recent PrepMD Webinar a panel discussion was held to share best practices to address the common challenges on cardiac device remote monitoring programs. The panel discussion was led by Rob Lerman, MD, CMO, along with three CCDS-certificated leaders from the  Kent Seckinger, CCDS, PrepMD 4+years, cardiac device space for 20 years, working split half between the device industry for manufacturers and the other half working for a large device clinic.
Kent Seckinger, CCDS, PrepMD 4+years, cardiac device space for 20 years, working split half between the device industry for manufacturers and the other half working for a large device clinic. Brianne Terrell, RN, CCDS, PrepMD 1 year, device clinic for about 10 years working in support of device implantation, patient consultation, perioperative device management, in-clinic follow up, and remote monitoring.
Brianne Terrell, RN, CCDS, PrepMD 1 year, device clinic for about 10 years working in support of device implantation, patient consultation, perioperative device management, in-clinic follow up, and remote monitoring.  Janet Cedric, CCDS, worked at Prepmd 4.5+ years and in the cardiac space for about 24 years. I’ve managed and started up device clinics.
Janet Cedric, CCDS, worked at Prepmd 4.5+ years and in the cardiac space for about 24 years. I’ve managed and started up device clinics. 
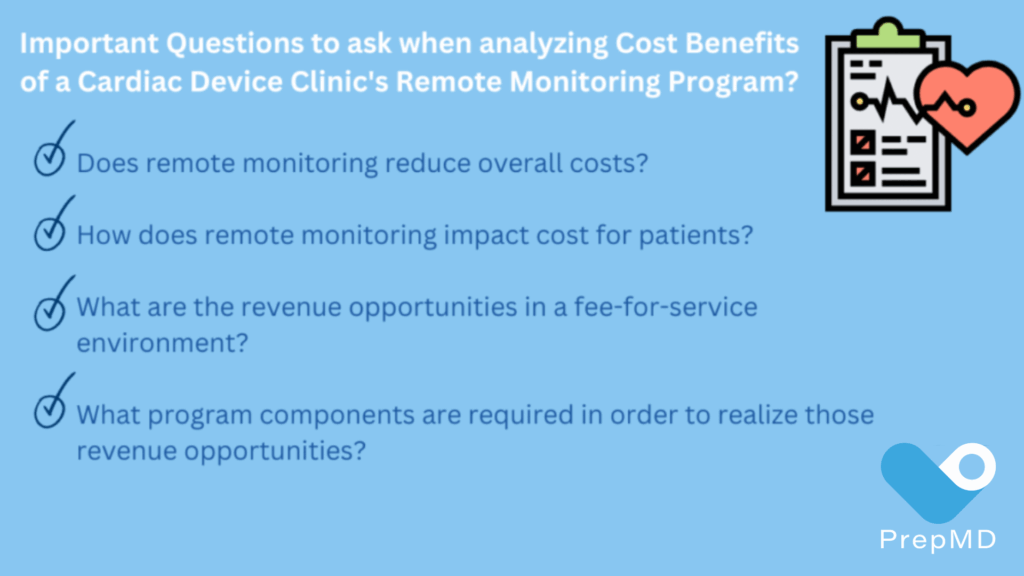
 Greg O’Neal, PrepMD Director of Product & Business Development explained, “In general, we find that many clinics running remote monitoring programs monitor patients less frequently than optimal. This highlights the discrepancy between the ideal monitoring frequency and the actual practices in clinics. The typical reimbursement is often less than 50% of the optimal.”
Greg O’Neal, PrepMD Director of Product & Business Development explained, “In general, we find that many clinics running remote monitoring programs monitor patients less frequently than optimal. This highlights the discrepancy between the ideal monitoring frequency and the actual practices in clinics. The typical reimbursement is often less than 50% of the optimal.”
 “Setting correct intervals, whether manual or automatic scheduling, in Boston Scientific, Medtronic Carelink, and St. Jude/Merlin/Abbott patient profiles can serve as a resource when determining the best dates for upcoming office visit device checks.”
“Setting correct intervals, whether manual or automatic scheduling, in Boston Scientific, Medtronic Carelink, and St. Jude/Merlin/Abbott patient profiles can serve as a resource when determining the best dates for upcoming office visit device checks.”