Watch Video
For Episode 4 of the PrepMD Webinar Series on remote monitoring for cardiac implantable electronic devices (CIED), Dr. Robert Lerman, PrepMD CMO spoke with Jason Clyne, Regional Economics Manager for Medtronic CRM about coding, billing, and reimbursement for cardiac rhythm management devices.

Highlights of the PrepMD and Medtronic conversation are below:

Lerman: Jason, I’m really excited to have you with us today. Can you tell us a little bit about what you do as a Regional Economics Manager?
 Clyne: Within Medtronic I focus on cardiac rhythm management- the ablation side, certainly pacemakers, ICDs, and cardiac diagnostics such as Linq as well as some of our other portfolios such as Tyrex. My conversations tend to be looking upstream at some of the different tools we have in the market access space and trying to uncover what that population of patients looks like, down to the point of service or procedure- coding, coverage, and payment scenarios. I also speak to the downstream value and all the great clinical outcomes that Medtronic provides as well as the great economic outcomes that accompany those clinical outcomes.
Clyne: Within Medtronic I focus on cardiac rhythm management- the ablation side, certainly pacemakers, ICDs, and cardiac diagnostics such as Linq as well as some of our other portfolios such as Tyrex. My conversations tend to be looking upstream at some of the different tools we have in the market access space and trying to uncover what that population of patients looks like, down to the point of service or procedure- coding, coverage, and payment scenarios. I also speak to the downstream value and all the great clinical outcomes that Medtronic provides as well as the great economic outcomes that accompany those clinical outcomes.
Lerman: Thanks, Jason. So here are a few key concepts that are important. The billing and coding requirements that we’re going to review don’t tell you how often device checks can be done. It is important that those decisions are governed by medical necessity as determined by the provider. We don’t even have control over the frequency of RM transmissions,- even clinicians and 3rd party companies don’t always control the frequency of patient-initiated or alert-generated transmissions. However, we DO have control over how often and for what we bill!
Second, this webinar will focus on traditional fee-for-service Medicare requirements and reimbursement. Even within traditional Medicare, there may be local coverage decisions and different approaches taken by different Medicare Administrative Contractors – or MACs. Additionally, Medicare Advantage, Medicaid, and private payors may all have different requirements such prior authorizations. So always check with your local MAC or payor for detail and requirements for your location.
Before we get into any details, please take a look at the PrepMD and Medtronic disclaimers below1,2 Essentially, the information presented is for information only and does not constitute legal advice or recommendations. Final responsibility for billing and coding is with the provider. While we have tried very hard to provide current and accurate information, even Medicare regulations change frequently, so again please contact your Medicare contractor, other payors, reimbursement specialists, and/or legal counsel for interpretation of coding, coverage, and payment policies.
Clyne: We’re certainly going to have some great conversations but again, not providing any legal advice, and we’re not recommending any clinical practice. That’s up to you the provider at home to constitute for your patients.
Lerman: We’re going to be talking mostly about Medicare rules and regulations. Medicare is a federal health insurance program for people who are predominantly 65 years of age or older. A Medicare Administrative Contractor or MAC is a private healthcare insurer that’s actually been awarded a geographic jurisdiction to process Medicare claims for their fee for service beneficiaries. Medicare relies on a network of MACs to serve as the primary operational contact between the fee for service program and healthcare providers. The MACs have a fair amount of latitude, not only to process claims, but to establish local coverage determinations called LCDs, as well as to review claims and medical records when appropriate. Which is why when say when in doubt to consult your local MAC, that’s what we’re talking about.
Keep in mind that Medicare has a variety of payment programs with different rules and reimbursement policies. Today we are focusing on the Physician Payment program. In this program, payments are made to physicians based on the Medicare Physician Fee Schedule which is updated at least annually on January 1. If you’re working in a hospital or Ambulatory Surgical Center, there are different payments systems and reimbursements differ.
There are some basic questions that you should ask when thinking about billing for CIED monitoring:
- What kind of devices are being monitored?
- Where is the service being performed?
- Should the service be billed globally or as separate technical and professional components?
- Who is performing the technical and professional components? Are modifiers necessary?
- What procedures are performed and what are the corresponding CPTâ codes?
- Are the services billable based on timing requirements?
So Jason, how often should CIEDs be monitored?
Clyne: It ultimately goes back to the provider. The provider knows the medical history, the indication for the device, and what follow-up routine is the best fit for a given patient. That’s where the guidance should start. What we’ll talk about now are guidelines, not mandates, but they help develop a routine for your clinic.
CMS has put out a national coverage determination for pacemakers, but note that it hasn’t been updated since 1984. It speaks to routine and asymptomatic management, that being one device evaluation per year for single chamber pacemakers and one every six months for dual chamber devices. Place of service is not specified. Some of the Medicare Administrative Contractors have started to put in some further language to help clarify, likely because there have been a lot of changes in our therapeutics since 1984. So for example we have a local coverage determination from Novitas for pacemakers that acknowledges that for symptomatic patients, the CMS guidance for routine follow-up can be combined with either remote or in-person follow-up with a reasonable frequency when medically necessary. We certainly advise that you look at your local guidance from your local Medicare Administrative Contractor. Also from a CPT® code perspective, the CPT® codes have finite guidelines, but from a remote monitoring standpoint we’re really looking at once every 90 days, a period of time that we’re going to monitor this.
The societies provide some further guidance. HRS updated their guidelines in 2015 and there may be an eventual change to this in the future. But the guidelines speak to at least one in-office transmission per year versus remote transmissions on the pacemaker side anywhere from every 3-12 months. So again, there is some variability there and the same applies on the ICD side with every 3-6 months, so there is some leeway there but at the same time some guidance as to how these patients should be managed.
Lerman: I think it is important to reinforce that the national coverage decision from CMS on pacemakers hasn’t been updated since 1984, which we know predates the modern era of remote monitoring, and they provided no guidance on ICDs at all. So as Jason pointed out, we have to rely on some of the local MACs decisions as well as the CPT® code guidance and that from the societies. We seem to get along pretty well, but it is interesting that CMS hasn’t made a national update in quite some time. In addition to the timing requirements, which we’ll discuss in further detail, there are some additional Medicare requirements around documentation and physician supervision. Jason, can you talk about some of those?
Clyne: Device interrogation whether remote or in-person is a diagnostic test. Like any diagnostic test being performed it requires a written order. The order needs to originate from the practitioner who uses the results to treat the patient. The patient medical record needs to clearly document the practitioner’s intent that the test be performed. In addition, medical necessity documentation is important, and this will come into play later when we discuss heart failure diagnostics and implantable physiological monitoring. Patient history and indication for the device can be utilized, but then specific to the individual test, what is the reasoning for ordering the test? What findings are being sought, and what are the results of those tests and how will they be used to manage the patient’s clinical issues? Each parameter tested and the results should be maintained in the medical record.
The next question to be addressed, whether the diagnostic tests are remote or in-person interrogation, is what kind of supervision is required? Most of the time it is a technician or a nurse that is completing the interrogation, whether in-person or remote. From a remote monitoring perspective, all that is required is general supervision. General supervision occurs when the procedure is provided under the supervising practitioner’s overall direction and control, but the supervising practitioner’s presence is not required during the performance of the procedure. The supervising physician is responsible for ensuring that there is proper training for the non-physician personnel that is performing the diagnostic test and that the equipment is maintained and proper supplies are provided.
The in-person interrogation is a different story, as now there is a patient in front of us, and maybe there is an opportunity for medical intervention as needed. So now there is a need for direct supervision. That direct supervision can be provided by a physician or now, a non-physician provider (NPP) such as a nurse practitioner or PA. They don’t need to be specifically in the room with you, but they should be close by in order to perform medical intervention if needed. A question arises for a hospital-based clinic that what if the physician is in the cath lab performing a procedure? Even though they are in the same building, if they are not immediately available to provide assistance and direction, then it does not qualify as direct supervision.
Lerman: The general supervision requirements for remote are what allows third party companies to participate in remote monitoring, because they can be done under the general supervision of the physician, who is not required to be in the same facility.
Clyne: That’s right.
Lerman: One of the things that differentiates in-person device checks from remote device checks is the concept of whether they are billed based upon global CPT® codes or individual technical and professional codes. For in-person checks, global codes exist, which encompass both the technical and professional components. If you are only reporting one of the professional or technical codes, a modifier is used. For example, if you are only billing the professional component, you would add a -26 modifier to the global code, and if you are only reporting the technical component, you would add a -TC modifier. One example of where these modifiers might be used is if an industry representative is performing the technical component of the in-person check. In that situation, the appropriate billing for the clinic or the physician is the -26 modifier for the professional component only.
On the remote side it is largely different. With one exception there are separate technical and professional CPT® codes. Third-party companies will frequently perform the technical component under general supervision, while the clinic practitioners perform the professional component of the evaluation. It is important to note that remote CPT® codes are appropriate whenever a patient is not physically at a healthcare facility to receive this service. Jason, can you help us better understand some of the details that distinguish the professional component from the technical component?
Clyne: The professional component is that physician’s interpretation of the diagnostic test performed and all findings included in a written report as well as relevant clinical issues. For in-person monitoring services it also includes all components of supervision of the diagnostic testing. The technical component can include a number of things, including the technician or nurse receiving and downloading the data and performing technical interpretation and distributing the results. The technical component includes all non-physician work performed, including the cost of administrative personnel, capital equipment and facility costs, and related malpractice expenses. One would think that the reimbursement would be heavily weighted towards the professional because that’s where a lot of the interpretation is being done, but there is a lot of work on the technical side that goes on behind the scenes.
——————————————————————————————————————————————
In part two of Remote Monitoring Billing and Coding we’ll discuss the individual remote monitoring CPT® codes, the concept and rules behind monitoring time intervals, and how dates of service variations create challenges for billing compliance.
1 PrepMD Disclaimer: PrepMD provides this information for general information purposes only. It does not constitute PrepMD makes no guarantee that the use of this information will prevent differences of opinion or viewed as instructions for selecting any particular code. Please contact your Medicare contractor, other payers, reimbursement specialists, and/or legal counsel for interpretation of coding, coverage and payment policies.
This document provides assistance for FDA approved or cleared indications.
CPT® copyright 2022 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. Applicable FARS/DFARS restrictions apply to government use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for the data contained or not contained herein.
2 Medtronic Disclaimer: Medtronic provides this information for your convenience only. It does not constitute legal advice or a recommendation regarding clinical practice. Information provided is gathered from third-party sources and is subject to change without notice due to frequently changing laws, rules and regulations. The provider has the responsibility to determine medical necessity and to submit appropriate codes and charges for care provided. Medtronic makes no guarantee that the use of this information will prevent differences of opinion or disputes with Medicare or other payers as to the correct form of billing or the amount that will be paid to providers of service. Please contact your Medicare contractor, other payers, reimbursement specialists and/or legal counsel for interpretation of coding, coverage and payment policies. This document provides assistance for FDA approved or cleared indications. Where reimbursement is sought for use of a product that may be inconsistent with, or not expressly specified in, the FDA cleared or approved labeling (e.g., instructions for use, operator’s manual or package insert), consult with your billing advisors or payers on handling such billing issues. Some payers may have policies that make it inappropriate to submit claims for such items or related service.
CPT copyright 2021 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. Applicable FARS/DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or i





 Cardiac Device Clinic Needs to Hire and Train Staff: The Device Clinic Manager feels as if the recruiting,hiring and training process is never complete. Finding staff that is trained and clinically ready to handle remote monitoring and in-clinic patient care is a tall order. Even after hiring competent clinic staff a Device Clinic Manager may have additional clinic staff in need of training.
Cardiac Device Clinic Needs to Hire and Train Staff: The Device Clinic Manager feels as if the recruiting,hiring and training process is never complete. Finding staff that is trained and clinically ready to handle remote monitoring and in-clinic patient care is a tall order. Even after hiring competent clinic staff a Device Clinic Manager may have additional clinic staff in need of training. 




 Clyne: Within Medtronic I focus on cardiac rhythm management- the ablation side, certainly pacemakers, ICDs, and cardiac diagnostics such as Linq as well as some of our other portfolios such as Tyrex. My conversations tend to be looking upstream at some of the different tools we have in the market access space and trying to uncover what that population of patients looks like, down to the point of service or procedure- coding, coverage, and payment scenarios. I also speak to the downstream value and all the great clinical outcomes that Medtronic provides as well as the great economic outcomes that accompany those clinical outcomes.
Clyne: Within Medtronic I focus on cardiac rhythm management- the ablation side, certainly pacemakers, ICDs, and cardiac diagnostics such as Linq as well as some of our other portfolios such as Tyrex. My conversations tend to be looking upstream at some of the different tools we have in the market access space and trying to uncover what that population of patients looks like, down to the point of service or procedure- coding, coverage, and payment scenarios. I also speak to the downstream value and all the great clinical outcomes that Medtronic provides as well as the great economic outcomes that accompany those clinical outcomes.
 “Post-op when the device is implanted, the patient has a great deal of information being thrown at them and it can be very overwhelming. Often, we find that at the wound check appointment the patient will be able to process information more effectively, especially if they are provided with helpful written documentation or FAQs to explain how their monitor works and what the frequency of transmissions will be.”
“Post-op when the device is implanted, the patient has a great deal of information being thrown at them and it can be very overwhelming. Often, we find that at the wound check appointment the patient will be able to process information more effectively, especially if they are provided with helpful written documentation or FAQs to explain how their monitor works and what the frequency of transmissions will be.”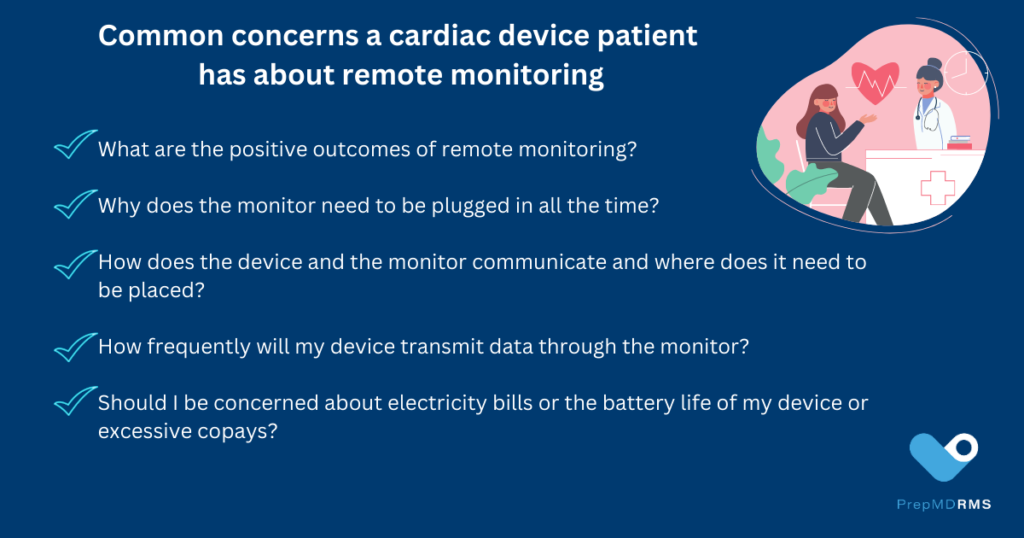

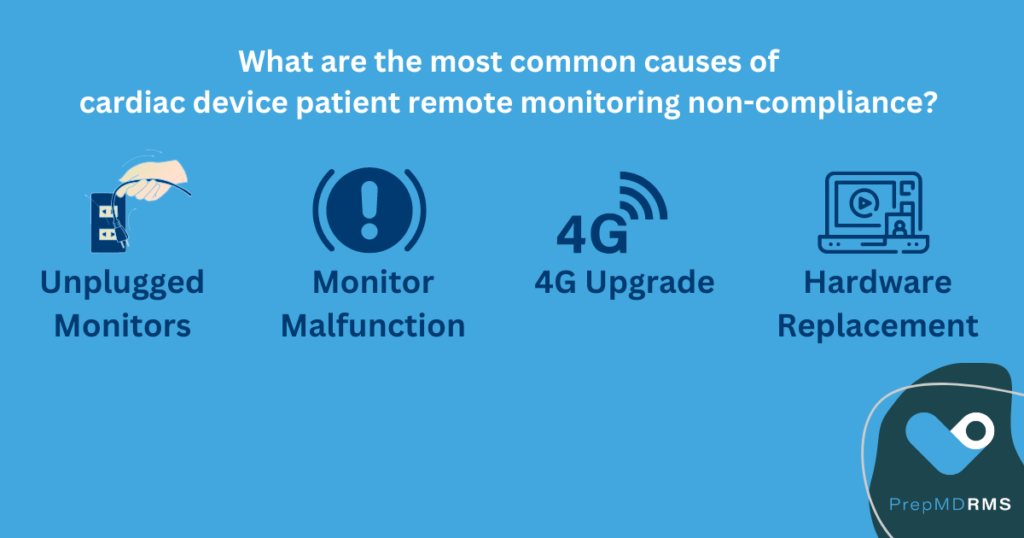
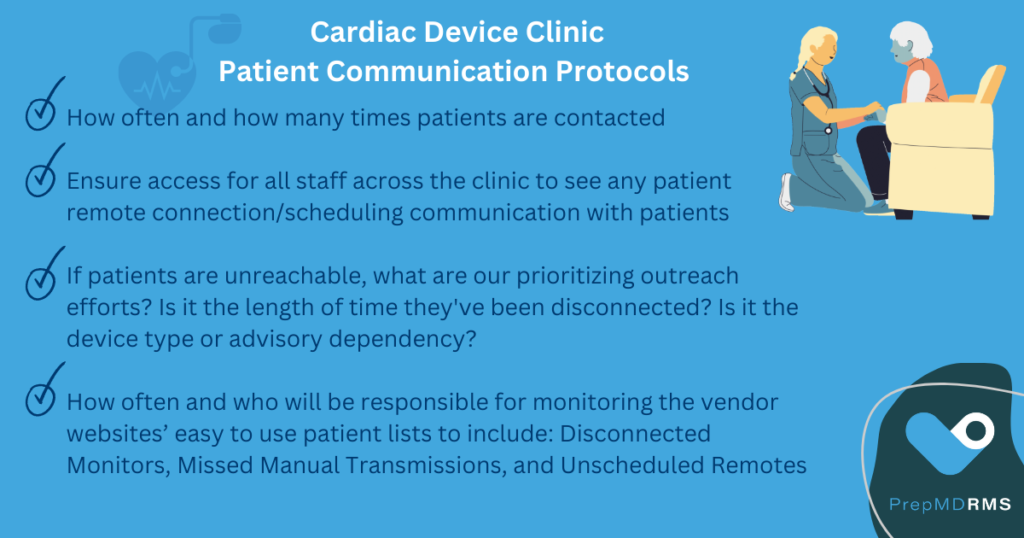
 “Whenever that’s the case, you may find that your disconnection rate is occurring more quickly than your recovery rate,” said Harris. She emphasized what she sees as the key ingredient to patient education success for patients at device clinics, “Clinics will be most effective if they have a dedicated person or team assigned to managing effective communication with patients to ensure remote monitoring compliance.”
“Whenever that’s the case, you may find that your disconnection rate is occurring more quickly than your recovery rate,” said Harris. She emphasized what she sees as the key ingredient to patient education success for patients at device clinics, “Clinics will be most effective if they have a dedicated person or team assigned to managing effective communication with patients to ensure remote monitoring compliance.”