Cardiac Device Patient Compliance – Keeping Patients Connected
Communication and Compliance: Patient Outreach Communication and CIED Remote Monitoring Compliance
In our last blog post, we discussed the potential clinical and economic benefits of remote monitoring for patients with Cardiovascular Implantable Electronic Devices (CIEDs). However, in order to realize these benefits there are multiple processes that need to be functioning at a high level. Several of those processes involve ensuring patient compliance, as both clinical and financial outcomes depend on consistent, reliable monitoring and reporting. Even though contemporary CIED transmitters and apps can be programmed to automatically communicate with devices and send transmission information to remote monitoring software platforms, disconnected monitors and the resultant missed transmissions are common. Scheduling of routine transmissions can also be time-consuming and confusing, with different processes for different manufacturers and devices. Troubleshooting disconnected monitors involves communication with patients which itself requires skill, patience, and understanding.
 At a recent PrepMD RMS educational webinar, Dr. Robert Lerman, Former Chief Medical Officer at PrepMD, moderated a discussion on Remote Monitoring Compliance and Patient Communication featuring two members of the PrepMD leadership team – Keith Nicholson, CCDS, PrepMD Business Operations Manager and Amy Harris, CCDS, Lead Patient Outreach Specialist.
At a recent PrepMD RMS educational webinar, Dr. Robert Lerman, Former Chief Medical Officer at PrepMD, moderated a discussion on Remote Monitoring Compliance and Patient Communication featuring two members of the PrepMD leadership team – Keith Nicholson, CCDS, PrepMD Business Operations Manager and Amy Harris, CCDS, Lead Patient Outreach Specialist.
Keith Nicholson kicked off the conversation by acknowledging that despite best efforts, it is inevitable that some patient monitors will become disconnected.
 “Regardless of best practices, disconnected patient monitors will happen. Patients unplug their monitor and forget about it, they move, or they need their device hardware upgraded. Every clinic should have a plan in place for how to deal with disconnected monitors.”
“Regardless of best practices, disconnected patient monitors will happen. Patients unplug their monitor and forget about it, they move, or they need their device hardware upgraded. Every clinic should have a plan in place for how to deal with disconnected monitors.”
Benefits of a dedicated team
Amy Harris discussed the most common approach to missed transmissions and disconnected monitors where every remote monitoring team member participates and just picks up the work when they can. With minimal staff time available, sometimes patients are simply referred to the manufacturer technical support phone line, but that can be fraught with challenges. Prompt selections or hold times may deter patients or family members, and technical issues with the monitors can sometimes require more in-depth troubleshooting just to diagnose the issue. Remote monitoring staff are typically busy keeping up with reading scheduled and unscheduled transmissions and alert escalations- reconnecting patients is often put on the back burner and addressed in piecemeal fashion.
 “Whenever that’s the case, you may find that your disconnection rate is occurring more quickly than your recovery rate,” said Harris. She emphasized what she sees as the key ingredient to patient education success for patients at device clinics, “Clinics will be most effective if they have a dedicated person or team assigned to managing effective communication with patients to ensure remote monitoring compliance.”
“Whenever that’s the case, you may find that your disconnection rate is occurring more quickly than your recovery rate,” said Harris. She emphasized what she sees as the key ingredient to patient education success for patients at device clinics, “Clinics will be most effective if they have a dedicated person or team assigned to managing effective communication with patients to ensure remote monitoring compliance.”
The inherent difficulties in getting patients reconnected, paired with the overall high volume of disconnected patients are common reasons to designate a dedicated individual or individuals to handle patient communication. This dedicated communication will ensure a better understanding of where each patient is within the process and helps prevent troubleshooting overlap or redundancy by limiting the number of individuals who are reaching out to patients.
“A dedicated staff member(s) will keep the patient communication process as brief and effective as possible for not just the patient, but clinical staff as well,” explained Harris.
Additionally, while on the phone with patients, dedicated outreach specialists can take the opportunity to fill-in any gaps in knowledge that patients may have about remote monitoring, update scheduling and vendor websites, or deactivate accounts of patients no longer being monitored.
Finally, there is a considerable amount of technical knowledge needed for the individual or individuals on the team who will be handling patient education and communication. There are at least 15 different monitoring systems across all the vendors, including bedside units and cell phone applications, and each monitor requires its own troubleshooting process. Familiarity is required in order to recognize each display of the various error codes or light sequences, as well as device compatibility and 4G connection requirements. Taking this wealth of complex technical knowledge and distilling only the required communication needed to accomplish what each patient needs can be complex and challenging.
What are the most common causes of patient non-compliance with remote monitoring?
- Unplugged monitors
- Monitor malfunction
- 4G upgrades
- Hardware replacement
Unplugged monitors are the most common cause of non-compliance. They can come loose from the power outlet by mistake. Those are an easy fix! Sometimes however, there are patients who don’t understand how remote monitoring works and may intentionally disconnect the power in between scheduled transmissions. Other issues may include poor placement within the room- such as under the bed- or patients going on vacation or out of town without their monitors. Here patient education is the key. Clearly when monitors malfunction or where there are new 4G connection requirements, detailed product knowledge is needed to troubleshoot. Sometimes our outreach specialists find it helpful to conference in patients and industry technical support staff but they stay on the call as well to facilitate communication. Currently patients who get new devices or replacement devices may have to wait on the shipment of back-ordered monitors. Education of patients on the use of smartphone monitoring apps when available can at times alleviate those supply chain issues, while other times they are unavoidable.
We have a dedicated team. Do we also need formal outreach protocols?
We recommend setting up a protocol with clinic preferences in mind for how to optimize the process, to clarify roles and responsibilities so that everyone is operating with the same understanding of who is doing what. Examples of the general protocol for patient communication may detail:
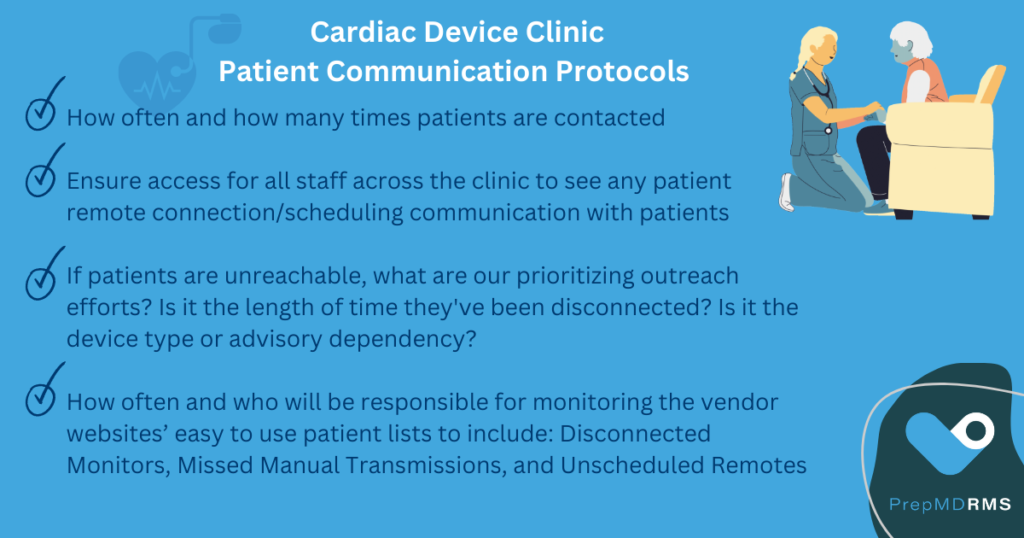
It is also important to properly document and keep tabs on patient outreach, including what was discussed with patients, and noting action and future plans such as patient education sessions.
Patients with Manual Transmissions: While most devices can be set up to send scheduled transmissions automatically, there are still some legacy devices out there that require patients to transmit manually. Some clinics will have to dedicate a staff member to calling the patient to walk them through the process of the manual transmission and explain to them what to expect and inform them of the next transmission date. Many times after doing that once, the patients will be able to handle the manual transmission on their own the next time. Some patients however, will need reminders before every scheduled transmission.
Once a backlog of disconnected monitors is cleared, what does maintenance look like?
Harris: “Once you get the [backlog] volume down to a manageable number, it’ll be much easier to just periodically scan the vendor websites for any connectivity issues or missed transmissions. You can also stay on top of upcoming schedules and proactively keep an eye on that. Depending on the size of the clinic…weekly checks would most likely be appropriate.”
What are some of the most surprising patient misconceptions encountered?
Harris: “I’ve heard some patients have a concern that their electricity bill is going to skyrocket or that even infrequent use of the remote monitor will drain the battery of their device or that the monitor being plugged in at the bedside is emitting harmful rays, or that they are incurring costs in the timeframe in between scheduled transmissions. These are times when education is provided much more thoroughly!”
Finally Nicholson was asked what kind of professional and personal traits he looks for in an outreach specialist in addition to the technical familiarity with the devices and monitors?
“Someone well versed in the EMR and kind of digging through and figuring out what’s going on , but also someone who is just kind of patient because some of these patients are frustrated and it’s not anyone’s fault, they want to get to the bottom of it. And sometimes just kind of having that calming presence to talk to the patient through is gonna be a lot more successful.”
Contact PrepMD to learn more about how they help address common CIED remote monitoring device clinic challenges with regard to patient communication and CIED Remote Monitoring compliance.


 Kent Seckinger, CCDS, PrepMD Customer Success Director, discussed how to best approach these common patient concerns. “What it really comes down to is patient education and transparency. Educating the device patients is critical to ensuring that they know that there are real benefits for them with remote monitoring. A discussion with each patient should include the specifics of the billing model and relevant regional reimbursement rates, and most importantly, an explanation of the clinical benefits realized with remote monitoring, such as reduction of hospitalizations and ER visits.”
Kent Seckinger, CCDS, PrepMD Customer Success Director, discussed how to best approach these common patient concerns. “What it really comes down to is patient education and transparency. Educating the device patients is critical to ensuring that they know that there are real benefits for them with remote monitoring. A discussion with each patient should include the specifics of the billing model and relevant regional reimbursement rates, and most importantly, an explanation of the clinical benefits realized with remote monitoring, such as reduction of hospitalizations and ER visits.” Greg O’Neal, PrepMD Director of Product & Business Development explained, “In general, we find that many clinics running remote monitoring programs monitor patients less frequently than optimal. This highlights the discrepancy between the ideal monitoring frequency and the actual practices in clinics. The typical reimbursement is often less than 50% of the optimal.”
Greg O’Neal, PrepMD Director of Product & Business Development explained, “In general, we find that many clinics running remote monitoring programs monitor patients less frequently than optimal. This highlights the discrepancy between the ideal monitoring frequency and the actual practices in clinics. The typical reimbursement is often less than 50% of the optimal.”
 “As a healthcare worker I realize that I seriously underestimate the impact on patients receiving an implantable cardioverter-defibrillator (ICD). Besides the patients I have the pleasure of caring for, I do not know anyone personally living with an ICD. Perhaps you do, but I am willing to bet a good majority of clinicians and device specialists do not know firsthand on what life is truly like for ICD patients.”
“As a healthcare worker I realize that I seriously underestimate the impact on patients receiving an implantable cardioverter-defibrillator (ICD). Besides the patients I have the pleasure of caring for, I do not know anyone personally living with an ICD. Perhaps you do, but I am willing to bet a good majority of clinicians and device specialists do not know firsthand on what life is truly like for ICD patients.” 
